Two years ago, a patient with a mysterious ailment was sent to Dr. Leon G. Smith, an infectious-disease (ID) specialist in Roseland. Practicing since 1956, Smith is generally regarded as the dean of the ID field in New Jersey. The patient had what’s known as a fever of unknown origin (FUO). Besides examining the patient and ordering a series of preliminary blood tests, Smith took a detailed history, one of the key investigative tools of the ID specialist.
The patient, Smith learned during his questioning, was a runner whose favorite place to exercise was a farm he owned outside the city where he lived—a farm, it turned out, that was overrun by cats. In the course of his jogs through the fields, the man had on numerous occasions brushed up against or touched fences, posts, railings, and other so-called fomites—objects that can transmit infectious agents. Smith used this information, which had escaped other investigators, to pinpoint the cause of his patient’s mysterious fever: It was the parasitic disease toxoplasmosis, which can infect most warm-blooded animals but most commonly infects, and is spread by, cats. Smith treated his patient with a special antibiotic, and the condition cleared.
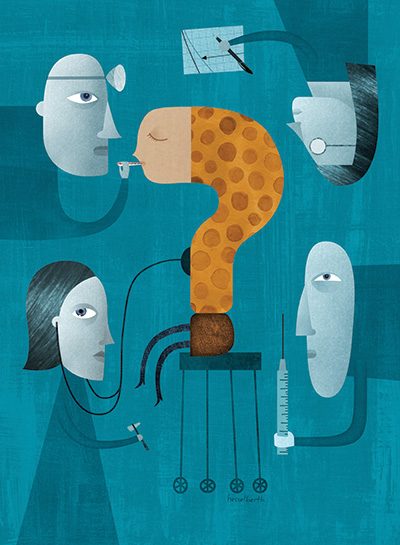
Welcome to the unpredictable, sometimes baffling world of infectious diseases—and to the unique group of specialists who investigate it. Part master diagnosticians, part medical sleuths, these specially trained doctors are often called upon to solve cases that baffle their colleagues. “We’re the Sherlock Holmeses of the medical world,” says Dr. Kathleen K. Casey, chief of infectious diseases at the Jersey Shore University Medical Center in Neptune.
Unlike specialists who focus on a single body part or system, ID doctors must cover the waterfront. “We’re not organ-based, since germs can affect any part of the body,” says Dr. Ronald Nahass, an infectious-disease doctor in Hillsborough. ID specialist Jerome F. Levine, of Hackensack University Medical Center, agrees: “You have to know the language of the entire spectrum and be able to deal with specialists in every field of medicine and surgery.” ID specialists must also have a more than passing acquaintance with epidemiology—the science of health and illness in specific populations. It doesn’t hurt, too, to have a keen sense of history, which sometimes plays a pivotal role in reaching a diagnosis.
“Several years ago, one of my interns mentioned to me that her 82-year-old grandmother in Israel had been experiencing a fever for a whole year,” says Smith, the Roseland specialist who is an avid student of history. “I asked where she was born, and when I heard Poland, I figured that she was probably raised in a Jewish ghetto, had been exposed as a child to epidemic louse-borne typhus, and now, after a long period of latency, the disease had recurred. This kind of recurring epidemic typhus is known as Brill-Zinsser disease.” Armed with the patient’s history, Smithmade the diagnosis over the phone.
Like all top detectives, ID specialists are also superb questioners and listeners, on the alert for that odd piece of data or seemingly trivial episode that may unlock an especially perplexing case. “We know that most doctors are busy, and sitting down for an hour to piece together a history isn’t something they have time to do,” says HUMC’s Levine. “But by the time patients comes to us, they’ve typically been through so much, and talking to them is what we do. You simply never know when something they say might be a tip-off.” That willingness to probe and listen without glancing at their watches catches many patients off guard. “They always say to me, ‘No one has ever talked to me this long or asked me these kinds of questions,’” says Jersey Shore’s Casey.
The patient history, lab results, epidemiological information, and historical perspective—each is an essential part of the ID doctor’s toolkit. “Anyone can come up with a diagnosis if he or she has an accurate and complete set of data,” says Levine with perhaps a bit too much modesty. In fact, as Levine himself goes on to explain, the data must be sorted, analyzed, and, if necessary, reevaluated. “I love problem solving and I love pattern recognition,” says Casey. “And in listening to the details of a patient’s story, I can start to tingle a little bit when I start to see what the differential diagnosis might be and how to figure it out.”
Recently, Levine treated a middle-aged woman with a pattern of non-healing ulcerated lesions, which had begun on her index finger, moved to her hand, and was progressing up her arm. By the time she visited Levine, her problem had been going on for six months. During this time, she’d been seen by a variety of doctors, who had treated her unsuccessfully with a “host of different antibiotics and antiviral agents,” Levine says. “Finally, someone said to her, ‘Maybe you should see an ID specialist.’”
At their first meeting, Levine started to probe. When did the symptoms start? When the woman told him six-months ago, he asked if she remembered anything out of the ordinary from the period immediately prior to her onset of symptoms. She recalled cutting her finger. And what was she doing when she cut her finger? The woman told him that she had been cleaning her fish tank. “As soon as I heard that, I thought about a specific infection, related to TB, called mycobacterium marinum,” Levine says. “As its name suggests, it’s an infection that’s often acquired from coming into contact with contaminated water in an aquarium or home fish tank.” Levine ordered a culture for the specific organism, confirmed his suspicions, and placed his patent on a regimen of antibiotics, which, within several weeks, caused the lesions on her hand and arm to begin to dry up and heal.
Mycobacterium marinum, of course, is no one’s idea of an everyday household bug; for this reason, the doctors who previously saw Levine’s patient may be forgiven for failing to reach an accurate diagnosis. But sometimes more common diseases also go undiagnosed, even when they show up in familiar guise.
Over the summer, for instance, a 21-year-old college student from central New Jersey walked into Nahass’s office. For the better part of the previous three weeks, she had shuttled back and forth between doctors, complaining initially of a painfully swollen right tonsil. Her primary-care physician examined her, said she had tonsillitis, and placed her on amoxicillin. After ten days, her other tonsil swelled. After a few more days, she returned to her doctor, who put her on a stronger antibiotic, along with a steroid. He also urged her to see her otolaryngologist (an ear, nose, and throat or ENT specialist) if her symptoms got worse, since it was likely, he explained, she would have to have her tonsils removed. A few days after this second visit, she started to develop lesions that progressed down her throat. “I couldn’t eat anything—I could only drink water,” she says. By this point, she had also developed lesions along the inner walls of her vagina, which at first she thought was probably a yeast infection.
That evening, still in pain, the student visited the emergency department of her local hospital. A female doctor there examined her genitals and throat; asked whether she was sexually active, which she said she was; and ordered blood tests. According to the student, the emergency doctor considered the possibility of herpes but concluded that “it really doesn’t look like that.” The young woman was reassured. “I didn’t worry about it because the emergency doctor didn’t seem concerned,” she says. She left the emergency department with Percocet to enable her to sleep and a mouthwash to numb her throat.
The following day, Saturday, she visited an ENT, who did more blood work in his office. On Monday, she went to a private lab for yet more blood tests, including a check for mononucleosis. Following these tests, she returned once again to her primary-care practice, where her regular doctor’s partner urged her to see an infectious-disease specialist.
She visited Nahass later that same day. Once in the exam room with his nurse-chaperone, Nahass had what he describes as an “aha” moment. “As soon as I lifted the sheet and examined her genitals, I said, ‘This is clearly a case of genital herpes, and it has spread to her mouth and throat.’” For Nahass, it wasn’t an “obscure diagnosis,” but it was one that could easily be missed.
In some instances, familiar diseases can present themselves strangely. As an STD, for instance, primary syphilis usually appears on the genitalia, but it can also show up on many other parts of the body. Similarly, tuberculosis typically attacks the lungs, but it can also affect other body parts, including the joints, where it disguises itself as arthritis.
In October 2009, recent Montclair State University graduate Daniel Stark, of Clifton, started visiting ID specialist Smith. Prior to seeing Smith, Stark, then 23, had spent a week in the hospital, followed by almost a month at the Kessler Institute for Rehabilitation in Saddle Brook. His hospital physicians had treated him—correctly—for infectious mononucleosis using an intravenously administered corticosteroid. But Stark’s symptoms weren’t garden variety for the disease. Besides the typical fever, fatigue, weight loss, and malaise, the young man couldn’t walk and was having increasing difficulty speaking. In fact, the doctors who treated him in the hospital suspected there was something else going on and even had their theories, which eventually proved accurate. But they “weren’t 100 percent sure,” says Stark. Following his week in the hospital, the young man was sent to Kessler, where he underwent intensive therapy to restore his speech and mobility. “What I experienced was similar to that of a stroke victim,” says Stark today. “I had to learn everything all over again.”
Following his release from Kessler, Stark was still moving around with the aid of a walker and had slurred speech. His father, a police officer, had heard of Smith’s reputation in the field of infectious diseases, and he was eager for his son to see the well-regarded physician. “From the day I came in with my walker, Dr. Smith was very welcoming, almost like a grandfather,” Stark says. “He ran tests from A to Z to pinpoint what I had—and what had caused it.” What Stark had, it turned out, was encephalitis, an acute inflammation of the brain and a rare complication of mononucleosis, and this was affecting his speech and gait.
“I couldn’t work during this period,” Stark says, “but Dr. Smith wanted me to stay mentally active, not just sit on the couch and watch TV.” The physician urged his patient to take up crossword puzzles. He also cautioned Stark against alcohol, which can cause inflammation and would retard his recovery. Finally, in order to strengthen his patient’s severely compromised immune system, Smith started him on a regimen of vitamins D and B12.
Last February, Stark was feeling well enough to return to work, a fact that stunned some of his early doctors, who had predicted a recovery of at least a year. (Stark is a salesman in an Apple computer store.) Five months after returning to work, he visited Smith for the last time. “In July, he gave me the stamp of approval that I was A-OK,” Stark says.
Kathleen Casey was also called upon recently to treat a disease that was manifesting itself in a decidedly odd manner. Several months ago, she explains, a man in his 70s showed up with his family in the Jersey Shore University Medical Center emergency department complaining of vague chest pains, low energy, and general malaise. Because of the man’s previous history of coronary artery disease, doctors admitted him into the emergency department in order to rule out cardiac ischemia, a condition in which the heart muscle or myocardium receives insufficient blood flow. Their plan was to administer a treadmill stress test.
His blood drawn, the man was placed on a stretcher to wait his turn on the treadmill. But in reviewing the patient’s complete blood count, the hematology tech noticed something strange—a clear abnormality. “The tech called the pathologist and he in turn called me,” says Casey, who realized almost immediately that “this guy had an infection, not cardiac disease.” The infection, it turned out, was babesiosis, a malaria-like parasitic disease, typically transmitted by ticks and probably acquired by this particular patient from mowing his lawn. “Chest pain is certainly not a common symptom of babesiosis,” says Casey. “Anyone more focused on the chest pain itself than on the blood count would miss it entirely.”
The emergency doctors had missed it, given the understandable focus on the man’s most obvious symptom. Says Casey: “In the emergency department, you’re supposed to keep people from dying from common things. And when an older person with a cardiac history comes in complaining of vague aches and pains—some of which are in the chest and shoulder region—the most obvious thing to think about is cardiac disease.”
Still, Casey knew that “the last thing [this infected and severely weakened patient] should be doing is taking a stress test. I looked in the computer, found where the man was, literally galloped to the cardiac-testing suite, and stopped the test.” Afterward, she called the patient’s attending physician to explain her diagnosis and say that, “I want to treat him and become an official part of the case.”
The clinical condition that’s often the biggest puzzle for ID specialists—and causes lots of other doctors to throw up their hands—is fever of unknown origin. “Fever is a common symptom of many diseases—the list is enormous, pages and pages in textbooks and articles,” says HUMC’s Levine. “But with FUO, the underlying disease that’s causing the fever isn’t known. How do you work that up?”
It’s precisely because of these diagnostic difficulties, Levine says, that many patients with FUO “just get put on antibiotics for a couple of days.” And that, he says, could “mask what’s really going on,” which poses a major clinical problem, especially in potentially fatal infections. “An infection of the heart valve—endocarditis—is one cause of FUO. If patients with underlying endocarditis are placed on an antibiotic before cultures of their blood have been made, doctors may never make the diagnosis.”
Not all cases of FUO, however, are genuine, which only adds to the condition’s diagnostic challenges. “First you have to document that they really are fevers,” says Smith, who has had many patients come into his office with pseudo fevers, which were likely the result of Munchausen syndrome, a psychiatric disorder in which someone feigns or self-induces a disease or psychological trauma in order to elicit sympathy or attention. To document that a fever is real, Smith orders a test to measure the blood’s sedimentation rate, an index of the amount of inflammation in the body. He also documents what type of fever the patient is experiencing—continuous, intermittent, or some other pattern.
Last summer, Nahass found himself puzzling over a case involving FUO. It concerned a 59-year-old man with a persistent fever, as high as 103 degrees, who had been first seen by his primary-care physician. After ordering some general blood tests, the doctor thought that his patient might have contracted one of several local tick-borne infectious diseases—anaplasmosis, ehrlichiosis, or Lyme. But after nearly two weeks on the antibiotic doxycycline, the man failed to get better. At this point, the doctor referred his patient to Nahass for evaluation.
During Nahass’s first meeting with him, the man complained, among other things, that there was something not quite right with his tongue. Concerned with making sense of his patient’s more apparent symptoms, Nahass noted the fact but didn’t ascribe much significance to it. But during one of the patient’s subsequent visits, Nahass, now accompanied by a student nurse-practitioner, had his attention redirected. “The NP was concerned about the patient’s tongue,” Nahass says. “It’s interesting how someone with less experience sometimes puts things together differently.”
The patient’s tongue problem, in fact, proved crucial to unlocking the mysteries of his case. After a consult with an oral surgeon and a scan of the man’s brain proved inconclusive, Nahass sent him for a CAT scan. The test revealed a mass in the patient’s abdomen that was affecting his liver and pancreas. Nahass feared pancreatic cancer, but a biopsy of the mass indicated the man had Burkitt’s lymphoma, a cancer of the lymphatic system. And though the brain scan had shown no brain involvement, a subsequent analysis of the patient’s spinal fluid showed the presence of cancer cells. These had traveled to the brain via the fluid and impinged on the patient’s twelth cranial nerve or hypoglossal—the very one that controls tongue movements. “After the patient’s first course or two of chemotherapy, his tongue went back to normal,” Nahass says.
Palsied tongues, tick-borne bugs, dangerous fish tanks, parasite-ridden cats—this is the world of the infectious disease sleuth, a world filled with almost as much unpredictability and mystery as, well, a good detective story. No wonder ID specialists love what they do.
“Never once in all my 28 years of practice have I ever been bored,” says Levine, echoing a refrain just about universal among his colleagues.
Contributing writer Wayne J. Guglielmo lives in Mahwah.
I was diagnosed of Herpes in 2014 and I have tried all possible means to get the cure but all to no avail, until i saw a post in a health forum about a Herbal Doctor(Dr Aloha) who prepares herbal medicine to cure all kind of diseases including Herpes,at first i doubted if it was real but decided to give it a try, when i contacted Dr Aloha through his Email: [email protected] he guided me and prepared a herbal medicine and sent it to me via courier Delivery service,when i received the package (herbal medicine) He gave me instructions on how to consume it,i started using it as instructed and i stooped getting outbreaks and the sores started vanishing,could you believe i was cured of this deadly virus within 10-14 days of using this REMEDY,couldn’t believe the healing at first until i went for a check-up,indeed i was tested negative to HERPES.Contact this great herbal Doctor today via Email: [email protected] and get cured permanently. or Call/Text: +1(312) 361-5917