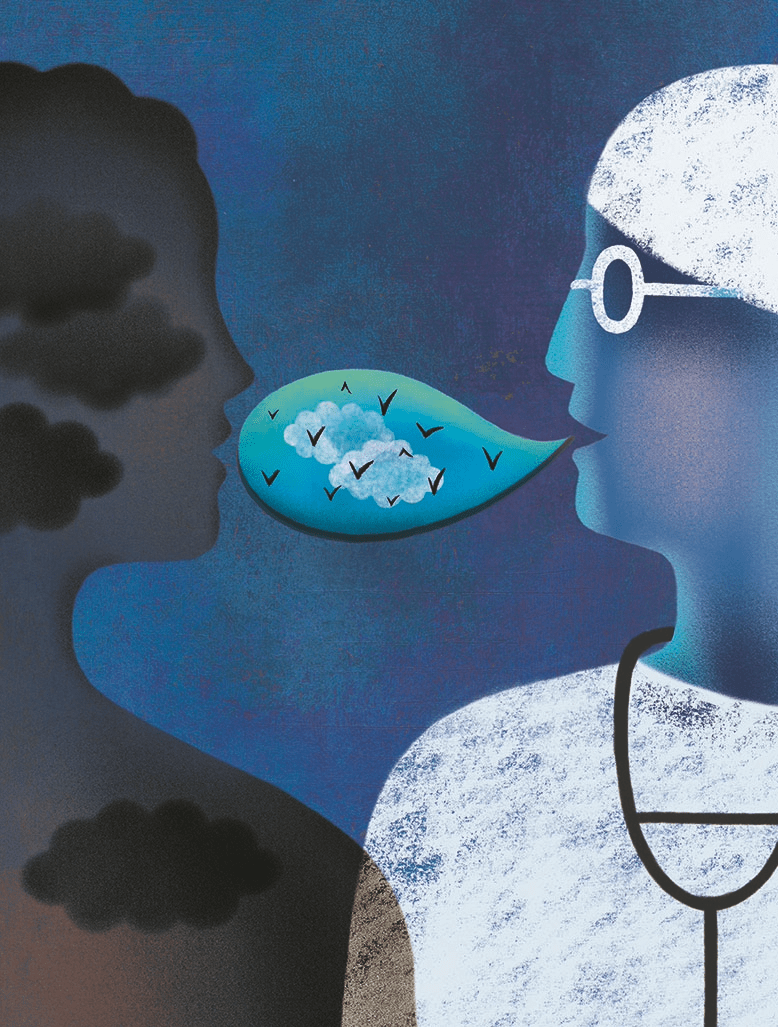
Illustration: Anna Godeassi
It’s a scene no one would want to endure. A brother and sister—David and Linda—are in a small hospital conference room, waiting to hear about their elderly mother’s worsening case of chronic obstructive pulmonary disease. David slumps in a chair, fixated on his cell phone. Linda paces, impatient for the news.
A medical resident enters the room and asks Linda to sit. She prefers to stand. David continues to obsess over his phone. The young doctor tries to engage them with a question: “Tell me a little bit from your perspective what you think is going on?” Linda takes a seat. David stares at his phone.
Ever so gently, the doctor breaks the news. “I’m afraid what I have to share is not good,” he tells them. Finally, David looks up. The resident describes two treatment options: one focused on relieving their mother’s discomfort, the second, a more aggressive approach. In either case, he makes clear, there’s no hope of saving the elderly patient.
Faced with the bleak prognosis, the siblings begin to argue, firing off accusations of blame and indifference at each other. The doctor gives them space to vent, then reminds them why they are there. “I want to do what’s best for your mother and for you,” he says, then asks, “does that sound good to you?”
At last, the reality sinks in. Their mother is dying. Both siblings break down in tears.
Buy our November 2023 issue here. Cover photo: Brad Trent
While the scene is all too realistic, David and Linda are, in fact, paid actors. Going into the scene, they had been directed to improvise whatever reactions they felt, from sadness to anger, as the young doctor described their imaginary mother’s fate.
“When it was over, the actors actually hugged the doctor,” says Liz Poret-Christ, managing director of the Orsini Way, the firm conducting the training session for medical residents. “That doctor was naturally amazing,” says Poret-Christ. However, she adds, “Communication skills like that are very unusual.”
In videos of other scenes, newly minted doctors with lesser skills appear as detached, insensitive or ill prepared. For these individuals, training in what is known as compassionate communication can be essential, covering such challenges as breaking bad news to patients and their families, as well as the difficult task of discussing medical mistakes.
Such training is part of the compassionate care—also called humanism—curriculum that has become standard at most medical schools. Simulations using trained actors are typical. Many hospitals provide similar training for their medical residents, either using internal resources or an outside coaching firm, such as the Orsini Way.
[RELATED: New Jersey’s Top Doctors]
Dr. Tanganyika Barnes, who runs the residency program at Englewood Hospital, defines compassionate care as “treating every patient as if they were a family member.”
This ideal—the ability of medical professionals to connect on a human level with their patients—is not new. It’s often thought of as bedside manner. For many practitioners, the promise of that connection draws them to medicine in the first place.
“It’s at the fundamental core of being a physician to really connect with people and to take care of them and to get to know who they are,” says Dr. Manasa Ayyala, an internal medicine specialist and director of the Healthcare Foundation Center for Humanism and Medicine at Rutgers New Jersey Medical School.
Unfortunately, the experts agree, the workplace stresses and technical strains of modern medicine have made such connections more difficult.
“Most people work for either a hospital-based group or another type of group,” says Ayyala. “So how,” she asks, “do you continue the personalized care?”
Being part of a hospital group or a large physicians’ group can put financial pressure on practitioners to limit their time with patients—often to 15 minutes, the modern standard. According to an Armstrong Institute for Patient Safety and Quality blog, “The 15-minute appointment arose not out of evidence that it improves patient outcomes, but out of production pressures—both the need to meet patient demand and to see enough patients to stay profitable.”
Yet patients, especially those facing a health crisis, yearn for their doctors’ time and attention. “When we see a doctor, we’re most vulnerable,” says Ayyala. “We want to be seen as people, to be treated with the respect and compassion we deserve.”
That’s where training can help. “We teach the biologic sciences with intentionality,” continues Ayyala, “but how do you teach compassion?”
TEACHING COMPASSION
At Rutgers New Jersey Medical School, the ideals of “kindness, compassion and humility” are taught as part of a formal course called Healing, Humanism, and Health Equity. Additionally, medical students can get involved at the school’s Center for Humanism and Medicine, where they can share personal experiences, learn from mentors, and get involved in community programs; some apply to be humanism fellows at the center and ultimately serve as role models for fellow students.
The relatively new Hackensack Meridian School of Medicine, which welcomed its first students in 2018, puts humanism at the heart of the curriculum, says Dr. Miriam Hoffman, vice dean of academic affairs. That starts with communication skills, which Hoffman defines as “the skills needed to build a collaborative doctor-patient relationship.”
Dr. Stephen Trzeciak, chief of medicine at Cooper University Health Care and professor and chair of medicine at Rowan University’s Cooper Medical School, says such skills can not only be taught, but can be beneficial for patients and caregivers alike. Compassionate care, he says, even has a financial benefit.
Trzeciak literally cowrote the book on the subject (with fellow Cooper doctor Anthony Mazzarelli). Their volume, Compassionomics (Studer Group, 2019), analyzed hundreds of scientific abstracts and research papers “to test the hypothesis that compassion matters,” says Trzeciak. Their conclusion: “When you deliver your care with compassion,” says Trzeciak, “you can actually have better outcomes for patients.”
[RELATED: NJ Doctors Wrote a Book on the Healing Power of Compassion]
Patients who believe their doctors personally care about them are “measurably more likely” to take their medicine, follow treatment recommendations, and come back for follow-up appointments, says Trzeciak.
Yet the ability to communicate compassionately can’t be taken for granted. “It used to be an assumed thing that you knew how to talk to patients,” says Hoffman. Or, as Trzeciak puts it, “Compassion was thought to be a-nice-to-have, sort of like the cherry on top of the sundae.”
That has changed. Today, says Hoffman, learning how to “establish a relationship founded on trust, where the patient is a partner” is central to medical education. “The acquisition of these skills,” she adds, “it’s not an afterthought.”
In Hoffman’s view, technology can foil such relationship building. “My grandfather was a general practitioner in the Bronx,” she relates. “The majority of his time was being with people. What’s the majority of a physician’s time now? It’s with the computer. It’s trying to find the best evidence, it’s looking for data, it’s looking for test results. That reality has created this need.”
But Trzeciak isn’t buying the excuse that today’s doctors lack the time for compassion. He cites a Johns Hopkins University School of Hygiene and Public Health study published in 1999 in the Journal of Clinical Oncology. Among other conclusions, the study found it only takes about 40 seconds for a physician to express “enhanced compassion.”
In other words, says Trzeciak, “you can go through your day with brusque efficiency, letting everybody know just how busy you are, or you can treat people with compassion. And if I held a stopwatch to you, it’d be the same thing.”
THE WHOLE PICTURE
Training in compassion often exists alongside exercises to raise awareness about unconscious biases, including preconceived notions based on a patient’s race, religion, gender or socioeconomic status. Related training focuses on facilitating better understanding of patients with rare diseases or other types of minority groups.
[RELATED: NJ Nonprofit Advocates for Patients With Rare Diseases]
At Rutgers New Jersey Medical School, the Healing, Humanism, and Health Equity coursework includes training in compassionate care. At Cooper, it’s called Foundations of Medical Practice. At Hackensack Meridian, humanism is woven throughout the curriculum.
All of these schools use professional actors in simulations as part of the training. This can include training in breaking bad news and other difficult scenarios. As with all simulations, the students receive immediate feedback from faculty and from the actors, who typically are referred to as standardized patients.
At Hackensack Meridian, simulations include trauma care, life-altering situations (such as delivering a cancer diagnosis) and end-of-life discussions. The school also hosts panels with members of the community, such as military veterans or persons with disabilities—with each group discussing “the challenges they face in establishing a trusting relationship,” Hoffman explains.
By connecting with members of the community, students learn, “It’s not just what I write on my prescription pad,” says Hoffman. “It’s what’s going on in your home, the stressors of your family members, what’s in your physical, built environment.”
Compassion is also a part of the curriculum for other prospective health professionals. Seton Hall University’s School of Health and Medical Sciences includes a college of nursing as well as graduate programs for aspiring physician assistants, occupational therapists, physical therapists, speech language pathologists and others.
Seton Hall has about 50 professional actors “trained in simulation case portrayal and debriefing” who are used as standardized patients, says Jennifer McCarthy, a clinical associate professor and director of clinical simulation at the School of Health and Medical Sciences. In simulations, the actors help students deal with breaking bad news or other difficult conversations on topics such as substance use disorder, diet and exercise.
Students, says McCarthy, “are thirsty for the verbal feedback from their patients and the desire to grow. I believe it’s a byproduct of this technology world. We spend so much time with our head down in a phone or on a computer or tablet.”
In some instances, the Seton Hall program—like many others—uses mannequins for scenarios “where clinical intervention is needed,” says McCarthy. The mannequins have heart sounds for simulating cardiac procedures, for example. Medicine can be administered or chest compressions performed. To simulate patient-doctor communication, actors in a control room provide voices for the mannequins.
Compassionate care is also on the agenda at schools such as Drew University in Madison, which offers a master’s degree in medical humanities, health and society; and Montclair State University, which has an undergraduate major in medical humanities.
CONTINUING EDUCATION
For many new physicians, training in compassionate care continues during their hospital residencies. At Englewood Hospital, first-year residents receive training in what residency director Barnes calls “difficult discussions.” That includes learning “how to have appropriate conversations about giving patients a cancer diagnosis or telling them they have a terminal disease,” says Barnes.
The training resumes for third-year residents, with the focus on “reporting adverse events”—in common parlance, medical errors. To prepare for such instances, the residents are taught about “owning up and taking accountability,” Barnes says. The most common missteps, Barnes says, are the lack of a plan for a difficult discussion and the failure to provide the guidance that patients and families need to make tough decisions like prolonging life for the terminally ill.
For its simulations, Englewood Hospital relies on the Orsini Way to provide actors and facilitate feedback sessions. Dr. Anthony Orsini, a neonatologist who formerly practiced at the Goryeb Children’s Hospital at Morristown Medical Center, founded the for-profit Orsini Way and his Breaking Bad News training program in 2010. Other clients include Morristown Medical Center, Virtua Health and Summit Health.
The Orsini Way helps trainees develop a plan for tough conversations, says Poret-Christ. It teaches them to break news gently but clearly and to give patients and families space to react. Perhaps above all, medical residents are coached to assure patients and their families that they are committed to the patient’s care.
At Atlantic Health System, standardized patients are used to train medical staff “in how to effectively communicate in difficult situations,” says Jeffrey L. Levine, director of academic affairs. Other programs on the humanistic aspects of medicine rely on staff resources, Levine says. For example, at Morristown Medical Center and Overlook Medical Center, the family-medicine residency programs employ clinical social workers.
Like other medical institutions, Atlantic Health holds what are known as narrative medicine sessions that “draw on the study of art and literature to enhance health care providers’ listening and observation skills,” says Levine. There are also walking groups to help staff members destress, and a book club, Literature in Medicine, featuring literary accounts of experiences with illness.
Overlook even has a poet in residence, Thomas Dooley, who conducts mindfulness walks with cancer patients and staff. Among other initiatives, Dooley provides therapeutic, bedside writing opportunities for hospitalized patients and mentors cancer patients “who wish to develop and write their cancer story,” Levine says.
THE BEST MEDICINE
For Cooper’s Trzeciak, the benefits of compassionate care accrue to providers as well as patients. Compassion can even have a financial benefit for health care organizations.
“This has to do with burnout and people leaving their organizations or leaving the profession entirely,” he explains.
Compassionate care includes what Trzeciak and others call “self-care”—that is, how doctors care for themselves, as well as the ways health care professionals watch out for each other. A caring environment can reduce turnover, he explains, adding that “high churn of healthcare workers is the biggest expense” for an organization.
Compassion, Trzeciak concludes, “can be the best medicine for yourself. If you treat patients with compassion, you get the relationships that flow from that. Then you get all the good part about being in medicine, being in health care. It’s still a hard job, but it’s like a good tired, because you get the fulfilling part. If you don’t have that, if you don’t have those relationships, then all you’re left with is a really stressful job.”
Ken Schlager is the former editor of New Jersey Monthly and a frequent contributor.
No one knows New Jersey like we do. Sign up for one of our free newsletters here. Want a print magazine mailed to you? Purchase an issue from our online store.