The young woman in trauma bay 3 is a still and silent counterpoint to the frenetic activity that swirls around her. She was wheeled into the New Jersey Trauma Center at Newark’s University Hospital just after 7 pm on an unseasonably cold day in March. A pinging chorus of pagers had heralded her impending entrance: A priority-1 trauma was on the way.
To be declared a priority 1—the most serious level of trauma—a patient has to meet one of 15 criteria. None of them is anything you’d want to experience. They include “impalement injury”; “crushed, degloved, or mangled extremity”; “amputation at or proximal to wrist or ankle”; and—the criterion that this particular patient fulfills—“penetrating injuries to the head, neck, torso, and extremities proximal to elbow and knee.” In the young woman’s case, it was a gunshot wound, and one that would prove something of a medical mystery.

X-ray shows a bullet lodged near the trauma patient’s spine.
The 15-by-15-foot bay is separated from those on each side of it by a set of curtains offering what passes for privacy in this most un-private of realms. If you’re unlucky enough to suffer a sudden trauma, this is where you want to find yourself. The bay is equipped with virtually everything necessary to treat a patient presenting with severe or life-threatening injuries, from a cardiac monitor and a ventilator to surgical instruments for cracking a chest, stopping a bleed, or otherwise patching up the all-too-vulnerable human body.
Now, members of the trauma team rush into the bay from one of two doors at each end of the long, rectangular space. They gather around the woman’s bed like dancers assembling on a stage. Helmed by tonight’s attending trauma surgeon, Dr. Ziad Sifri, a trauma and critical care surgeon, the team comprises four residents and interns, two trauma nurses and several medical technicians. They do their jobs with the practiced assurance of professionals who’ve performed this ballet, or some variation of it, dozens, if not hundreds, of times before.
After an initial exam, a technician wheels in a portable X-ray machine and positions it over the patient. Just before he takes the first exposure, he clears the room with a single command: “X-ray.” The team backs away in unison as one of them calls out, “Cover your gonads,” adding a touch of gallows humor to the proceedings. With each new picture, they repeat the practiced moves, a tense line dance with its own internal grace. Tonight their audience, standing by the admitting desk a few yards away, includes the two female paramedics who brought in the patient and a couple of Newark police detectives with shaved heads, slightly rumpled suits, and the air of having been here and done this many times over.
The woman is stable—her pulse, temperature and blood pressure are within the normal range—but complaining of stomach pains, which is perplexing to the medical team because the X-rays show a bullet nestled up against the base of her vertebral column. When a bullet gets that close to the spine, paralysis is a significant risk, but that’s clearly not the case here because the patient was up and walking for a time after she was shot. At 7:15, Sifri sends her next door for a CAT scan in the hope of shedding additional light on her condition. The team disperses, and an employee from housekeeping replaces them, sweeping up bits of bandage and plastic packaging.
Case 1: Gunshot Wound
- An ambulance leaves the New Jersey Trauma Center at Newark’s University Hospital, which treats some 3,000 seriously injured patients a year.
- Dr. Ziad Sifri, a trauma and critical care surgeon, left, checks the patient for sensation in her lower extremities. Because initial X-rays indicate that a bullet is lodged next to her spine, paralysis is a concern.
- As the trauma team preps the patient for surgery, Sifri keeps an eye on the monitor for her vital signs.
- Sifri takes a breather at the nurses’ station while his team gets ready to move the victim. Part of his job is to make sure that the team is following protocol.
Welcome to a quiet night at one of New Jersey’s three Level I trauma centers. (The others are located within Robert Wood Johnson University Hospital in New Brunswick and Cooper Hospital/University Medical Center in Camden.) Level I centers are equipped to treat the most serious trauma patients, those at risk of death or loss of function. Like all three Level I centers in New Jersey, they’re generally part of a university-affiliated teaching hospital, with routine access to cutting-edge research. In addition, the state requires Level I centers to treat a minimum of 600 patients per year, since data indicates a strong correlation between patient outcomes and the number of procedures performed. University Hospital treats some 3,000 trauma patients each year, 2,000 of them serious enough to be admitted for additional treatment. (New Jersey also has seven Level II trauma centers, which are equipped to deal with serious trauma cases but may not be affiliated with teaching hospitals and are only required to treat 350 patients per year.)
Considering the Level I traffic, the center looks surprisingly small, but it’s highly functional. The 25-by-200-foot space has four contiguous trauma bays and one closed shock-trauma room, where the most severe cases are treated, plus a nursing station and a hallway facing the bays. Without making any special accommodations, like closing the ER or expanding into other hospital units, the center can handle five critically injured patients and another five with moderate injuries at any time. Any greater number could trigger the center’s mass-casualty plan, which involves clearing the emergency department, among other measures.
The center’s inner-city location dictates the type and severity of cases that get wheeled through its doors. “We see a lot more knives and guns than most places,” says Dr. Stephanie Bonne, a trauma surgeon who recently transferred to University Hospital from Washington University Medical Center in St. Louis. Her colleague, surgeon Anastasia Kunac—petite and visibly pregnant—agrees. “The amount of violence that we see,” she says, “is unusual.”
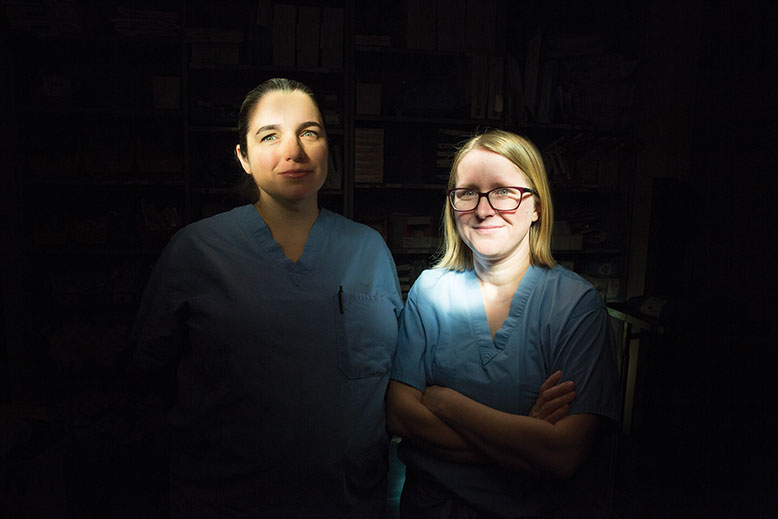
Trauma surgeons Anastasia Kunac, left, and Stephanie Bonne. For both women, starting their own families changed the way they approached the job. Photo by Fred R. Conrad
In fact, about a quarter of the center’s patients sustain damage from penetrating trauma—an injury in which a foreign object, like a bullet or a knife, enters the body. Most of the other injuries are so-called blunt trauma, caused by a non-penetrating object (say, a baseball bat) or collision with a blunt surface, such as a motor vehicle. A third of all the trauma cases seen at University are the result of interpersonal violence. The center also treats burn victims, usually those who have sustained traumatic injuries (after jumping from a window, for instance) in addition to the burns. Otherwise, most burn victims are taken to a dedicated burn center like St. Barnabas in Livingston, often after initial treatment for trauma at University.
Both Bonne and Kunac have young kids at home, and both admit that the job has made them overprotective of their family members. “There are things I don’t allow in my home,” says Bonne. “No trampolines, no motorcycles, no older parents on ladders. No aspirin, it thins the blood, you can bump your head and start a big bleed.” Her kids never ride their bikes without helmets. To get on their scooters, they also have to wear knee and elbow pads.
Spend some time in the center, and you can see where that caution comes from. Half an hour after the gunshot patient is moved down the hall for a CAT scan, two paramedics roll in another woman on a gurney. She is moaning loudly.
The patient was riding a motorcycle, the paramedics explain, when another vehicle cut her off, causing her to swerve and fall off the bike. Luckily, she was wearing a helmet, which may have prevented traumatic brain injury and even have saved her life. She’s already been given a dose of fentanyl, a powerful opiate painkiller, but she asks for another, and the trauma team, now assembled around her, complies. Her vital signs are stable, and she’s fully conscious, but all motorcycle-crash patients are considered traumas, since the lack of a protective “nest” (such as a car or truck) makes them particularly vulnerable to internal injuries.
One of the nurses cuts the patient out of her clothing. Because Sifri is upstairs in surgery, operating on the gunshot victim, Dr. Adam Fox, associate trauma medical director, steps in as team leader. The system is designed so that backup is always at hand. (In fact, Fox had been on his way home when he received the page to return—trauma surgeons are used to making sudden U-turns.)
Case 2: Motorcycle Accident
- Associate trauma medical director Adam Fox questions the patient to determine where she has pain, while his team takes her vital signs.
- The team gingerly rolls the patient onto her back to check for injuries.
- Fox confers with a junior surgical resident, while a technician X-rays the patient.
- Fox checks the X-rays. “I don’t see a whole lot of anything that could be causing her pain,” he notes.
- Fox checks on the status of a previous patient. Cases often overlap in the trauma center.
Fox is trying to determine the exact nature of the patient’s injury. “Is the pain in your neck?” he asks her. “Your back? Your hand?” She says no each time, so the team deftly turns her on her side, where they find a small bruise on her lower left flank. Fox calls for X-rays, then leaves to check on the gunshot victim.
Twenty minutes later, he’s back, with the earlier puzzle solved. Apparently, the gunshot victim is suffering from an injury to her pancreas—the source of her abdominal pain—and perhaps other organs as well (she’s still in surgery). But it seems there is no injury to the abdomen proper, and the bullet, which looked in the X-ray as though it were lying against her spine, is actually lodged in the muscles of her back. While that’s good news, it’s still unclear whether or not she’ll make it. On the other hand, the motorcycle-accident victim doesn’t appear to have sustained anything more serious than some deep contusions. Before she’s sent out for a CAT scan, she asks for her cell phone. “It’s always a good sign when people are able to use their phones,” notes Fox.
At 45, Fox has already seen a lifetime’s worth of motorcycle and gunshot traumas. He’s tall and boyish looking, but his face radiates confidence. In many ways, he’s the archetypal trauma surgeon, drawn to the field by challenges that most people—including most doctors—would try to avoid, including the pressure to make split-second, life-or-death decisions. “A patient comes in and you have to do so many different things—identify and fix the injury, stabilize the patient—all within 10 to 15 minutes,” he says. The demands can be brutal—Fox has just come off a week in which he worked 100 hours—but the adrenaline rush and the satisfaction of saving lives on a regular basis are addictive. Fox started out as a podiatrist but went back to med school to retrain as a trauma surgeon. “I wasn’t the kind of person who could sit in an office doing corns and bunions all day,” he says.
Like Fox, Bonne and Kunac acknowledge that the job is stressful, but say the stress is commensurate with its rewards. “You get to see terrible things happening,” says Bonne, “but you also know that if you weren’t here, it would be worse.” Kunac appreciates the opportunity for problem solving. “Trauma bay,” she says, “is one of the places where medicine is pure and simple. There are 15 people in the room, and everyone is focused on that one patient. There’s no consideration of his status, who he is, whether he’s a cop or a robber.”
“We’re trained to treat patients with very rudimentary information,” says Dr. David Livingston, chief of trauma surgery. Having spent 28 years at University Hospital, he’s the center’s paterfamilias, with deep-set eyes, a short, gray beard, and a gold hoop in his left ear. He admits to feeling parental about his staff. “My most important job,” he says, “is to take people like Dr. Bonne and Dr. Kunac and give them the space and the mentorship to fulfill their academic destinies.” He’s also tough, fast talking—anything but sentimental. “I tend to like very sick people,” he says, a statement that might sound perverse coming from someone else. But Livingston is passionate about the varied population he believes it’s his privilege to treat. “We have penetrating trauma, blunt trauma, children, old people,” he says. “We take care of everybody, all races, all ages.” The center also conducts regular drills in anticipation of mass-casualty events like the World Trade Center and Boston Marathon attacks. “We know how to lock down, evacuate the hospital, get hold of as many doctors as possible,” says Bonne.
The toughest part of the job isn’t necessarily dealing with injuries, but with their aftermath, especially if those injuries prove fatal. Two weeks earlier, Kunac had worked on a man in his early 20s who had been shot in the abdomen. When he came in, he had no pulse, but the team opened his chest and got his heart going again, then repaired the shredded blood vessels in his abdomen and transfused him to replace the blood he had lost. But he was extremely unstable, and his heart stopped repeatedly during surgery. Despite the team’s best efforts, he died in the OR. “When I broke the news to the family,” Kunac says, “his mother told me that we didn’t know what we were doing and that we had let her son die. Even as a mother of two, I can’t pretend to imagine her pain, but I wish she’d understood that I was grieving alongside her.”
“There are nights when we have to tell people three or four times that their kids—kids in their 20s—are dead,” says Fox. “Outside of oncology, we probably deal with more death than any other specialty.” Luckily, the saves outnumber the losses. Fox looks around at the trauma bay, gone quiet for a short period, and smiles. “This,” he says, “is my favorite place in the hospital.”
A week later, Fox is back in his favorite place examining a burn victim who, unlike most trauma patients, has walked into the center under his own steam. A nurse explains that he was brought here the night before, signed out against medical advice, and returned this evening at 7 o’clock. Behind the trauma-bay curtain, the patient is singing loudly. When Fox and one of the previous surgical fellows, Victor Ha, enter the bay to examine him, he admits that he’s on heroin—“for the pain,” he says. A nurse undresses him, revealing patchy, blistering burns that cover most of his body. Family members attacked him with a hot iron. Given the extent of his injuries, Fox determines that he should be transferred to a burn center for treatment and observation.
As a nurse picks up the phone to arrange the transfer, the patient starts to pull out his IV. He doesn’t want to go to the burn center and insists that he can take care of himself. The nurse attempts to calm him down—“We don’t have to have this standoff,” she says—but he’s adamant. In a last-ditch effort to keep him from leaving, Fox and Ha ask him the standard questions to determine whether he’s mentally fit to make medical decisions on his own behalf: the day of the week, the month, the year, the name of the current president, and finally, whether he’s depressed or suicidal. Unfortunately for Fox—and no doubt for the patient as well—he answers every question correctly and denies being either depressed or suicidal. “I can’t stop you from leaving,” Fox says. “but those burns can get infected and you can die. You don’t want to die, do you?”
Case 3: Burn
- Fox discusses his decision to transfer the patient—who has second-degree burns from a hot iron covering at least 20 percent of his body—to the burn center at St. Barnabas Medical Center, where he can receive more specialized care.
- Fox takes cell phone photos of the patient to send to St. Barnabas.
- The patient refuses transfer to the burn center so two surgical residents are called in to clean and bandage his burns.
- Members of the team refuel with a delivery of Thai food, eaten in the doctors’ lounge.
He doesn’t want to die, but he doesn’t want to spend several days in the hospital, either. Eventually, Fox convinces him to allow the team to at least clean and bandage his burns. He sends in a resident to take care of it, then utters an expletive. “It’s a crazy day,” he says.
Then again, it’s a Friday, and Friday nights often get crazy. That’s true of weekends in general, when people are more likely to do the things that land them in the trauma center, like drink, take drugs, get into fights and drive under the influence. And as the weather heats up, so does the center. Warm weather brings people outdoors. Kids ride their bikes, which sometimes take them into the path of an oncoming car. Adults ride motorcycles, exposing themselves to all manner of potential trauma. (According to a 2014 study by the Insurance Information Institute, motorcyclists are five times more likely than passenger-car occupants to be injured in an accident on the road, and 27 times more likely to die of those injuries.)
On the weekends, it’s especially important to take advantage of whatever downtime fate offers. After the burn victim is discharged, Fox goes to his office, the closest thing at the hospital to a home away from home. It’s outfitted with what he calls “my favorite purchase”: a futon capacious enough for his 6-foot frame. Like most trauma docs, he sleeps when—and where—he can. “I’m convinced that the stress of this particular specialty, along with the lack of sleep, takes years off your life,” he says. In fact, a 2014 study published in the Journal of Trauma and Acute Care Surgery found that 15 percent of trauma surgeons met the diagnostic criteria for PTSD and 40 percent showed symptoms of the disorder.
Forty minutes after the burn victim is discharged, the PA system announces the imminent arrival of a patient to trauma bed 4, and Fox lopes through the center’s doors just as first responders wheel in the patient, a middle-aged man found lying in the parking lot of a nearby restaurant, his face bloodied, complaining of head pain. Because head pain could indicate a traumatic brain injury, the EMTs decided to bring him to the trauma center instead of the emergency room. Like members of the hospital’s trauma team, emergency medical technicians and paramedics are trained to make life-and-death decisions on the fly. (Paramedics have more training—about 1,200 to 1,800 hours versus about 120 to 150 for EMTs—and are permitted to perform more medical procedures.) These first responders have to evaluate the patient’s condition, decide what initial treatments (if any) should be administered, and—perhaps most important—determine where the patient should be taken for treatment. If they ascertain that a patient is suffering from severe trauma, he or she will be taken to a certified trauma center, most likely the closest one, though it’s possible that if a center is particularly busy, it will instruct the ambulance crew to go elsewhere.
Case 4: Bicycle Accident
- The trauma team prepares to treat a cyclist who was impaled by one of his handlebars when his bike was sideswiped by a car.
- Led by Fox, the team discovers massive internal bleeding.
- To stanch the bleeding, the team inserts an inflatable compression balloon in the patient’s abdomen.
- With the trauma team’s work complete, the patient is rushed into surgery.
- A member of the housekeeping staff cleans up the trauma bay in preparation for the next patient.
If a patient is trapped and needs to be extricated, or if traffic threatens to make it difficult for an ambulance to get to a trauma center (Level I or II) within 30 minutes, there’s another option: medevac. In 1988, New Jersey instituted its first helicopter evacuation service for trauma victims, NorthSTAR (an acronym for Northern Shock-Trauma Air Rescue). Each of the four helicopters in the NorthSTAR fleet is manned by two New Jersey State Police pilots, a flight paramedic, and a flight nurse. Initially headquartered at University Hospital, the program moved its headquarters to the more centrally located Somerset Airport in 2005, although it maintains an alternate base at University Hospital’s roof level. NorthSTAR has answered a wild array of calls: an overturned military transport on the Jersey Turnpike, a police officer with multiple gunshot wounds, a Cub Scout leader mauled by a bear, a tourist who suffered a massive coronary at the Statue of Liberty and a small, plane crash. Paramedic Terry Hoben has been with the service since its inception, and like almost everyone in trauma care, he’s got a thing for adrenaline.
“I was intrigued by the challenge of taking care of a patient in a very short period of time,” he says. In a typical month, University will receive nine patients via NorthSTAR, although that number is likely to spike in the busier summer months. In his 28 years as a flight paramedic, Hoben has responded to hundreds of trauma calls. The worst calls, he says, are the ones involving kids. “We deal with those a lot,” Hoben says, “because kids are risk takers.” Spring is a particularly rough time for paramedics, both in the air and on the ground, because it’s prom season and, says Hoben, “something bad always happens during prom season.”
It was on a Friday night in July 2016 that Fox treated his own record number of traumas: 18 in a 12-hour period. But this evening, spring is only a day old, and the temperature is expected to dip below freezing by the small hours, presaging the possibility of a calm night. At the moment, a team of eight is working on the patient brought in from the parking lot. He doesn’t remember how he ended up there, but he does know the day of the week, the name of the hospital, and the president of the United States. As Fox watches, an intern checks the man’s condition. The intern asks the man to move his legs and his arms, to squeeze the intern’s fingers and push him away, to hug himself. He can do it all, a good sign. But, notes Fox, “blood on his head, altered mental status—that, until proven otherwise, is a traumatic brain injury.”
Fox doesn’t have time to expand on that thought because just then, his pager goes off. “Getting another one,” he says. “Kid struck by a car.” Dr. Tyrone Reyes, a pediatric attending from the ER, is called in, and five minutes later, at 10 pm, a paramedic wheels in a four-year-old boy. He’s tiny and scared, and the neck brace he’s wearing makes him look even smaller. At his side is a young man in a Yankees cap and a young woman who’s limping slightly. (They turn out to be his father and aunt.) When he’s settled in the bay, he starts to whimper, no doubt unnerved by the blue-gowned strangers hovering over him. Off to the side, Fox grabs a latex glove, blows it up, and starts drawing on it with a Sharpie. He walks over to the boy and hands him the glove, which, with its inked-in eyes, nose, and mouth, is the trauma center’s approximation of a toy. “Hey, buddy,” Fox asks, “want this?”
That sets off an even more furious round of crying as the team works to ascertain where, and how seriously, the boy is injured. It looks like he may have injuries to his pelvis. Fox calls for an X-ray. Meanwhile, the story emerges: The boy and his aunt were outside with neighbors when a car backed into them. She put herself between the boy and the car and, in doing so, she appears to have been injured as well. As she sobs, the paramedic walks over to her. “You did good,” he says. “You protected him.”
Fox asks if they can check her out. He tells her that her nephew is fine. “Everything we’re seeing indicates that there’s nothing life threatening,” he says. She goes to the boy’s bedside and gently touches his face. At about 10:15 pm, his mother and great-grandmother walk in. The two sisters embrace, crying.
Meanwhile, the man from the parking lot has been taken next door for a CAT scan. The little boy’s family are talking quietly, and he’s playing with the latex balloon, intently pulling on its swollen fingers. For a short time, the noise and tumult recede. The only sound is the rhythmic beeping of the monitors, the pulse of the trauma center.
At 10:50 pm, the man from the parking lot is wheeled back into trauma bay 2. A resident tries to flush his IV, and he objects. “Ow,” he says. “Stop.” She tells him she’s going to clean up his face, bending over him with a syringe. “That hurts, yo,” he tells her. Bits of blood-soaked gauze fall to the floor. “All done, sir,” the doctor says, pulling off her mask.
Forty minutes later, two Newark police officers bring in an inmate from Northern State Prison. His head is bandaged, but he’s not a trauma patient. The center is often host to prisoners, even when they don’t present with trauma, because it’s smaller than the ER and usually less crowded. He and the cops engage in conversation behind the closed curtain. “Those bracelets do have to go back on,” one of them says, referring to the handcuffs that were removed during treatment. “Cory Booker is going to be president one day,” the prisoner says, apparently continuing a conversation begun on the way over.
Fox returns with good news: The boy is fine, just a little sore. A while later, his father carries him out of the center, trailing the rest of the family. Meanwhile, the prisoner is wheeled down the hall for a CAT scan. A nurse is on the computer, checking the basketball scores. Under the fluorescents, the place is a portrait of medical personnel in repose. As always, life in the trauma center tonight is made up of periods of tedium punctuated by bursts of controlled chaos. The next burst begins at 1:20 am when the calm is punctured by a page announcing a motorcycle accident, priority 1, ETA 1:40 am. The nurse logs off; Fox stands next to an empty trauma bay, ready. The night goes on.
Jersey’s Trauma Network
Level-I Trauma Centers
(part of a university-affiliated teaching hospitals; must treat a minimum of 600 patients per year)
Cooper Hospital/University Medical Center | Camden
Robert Wood Johnson University Hospital | New Brunswick
University Hospital | Newark
Level-II Trauma Centers
(not necessarily affiliated with a teaching hospital; must treat a minimum of 350 patients per year)
AtlantiCare Regional Medical Center | Atlantic City
Capital Health Regional Medical Center | Trenton
Hackensack University Medical Center | Hackensack
Jersey City Medical Center | Jersey City
Jersey Shore Medical Center | Neptune
Morristown Memorial Hospital | Morristown
St. Joseph’s Regional Medical Center | Paterson